Regenerative medicine might just have had a new tool added to its arsenal: Scientists have created tiny biological robots out of living human cells. Though they may be small, the self-assembling bots are mighty, with a study demonstrating their potential for healing and treating disease.
The team had already proven their biological robotics chops back in 2020 with the creation of Xenobots, made from frog embryonic cells. They even managed to design Xenobots so that they could reproduce in a way that no living animal or plant does, something that had never been seen before.
The researchers weren’t sure whether the incredible capabilities of the Xenobots were in some way down to their amphibious origins, so they wanted to find out if biobots could also be created from the cells of other organisms. And why not begin with humans?
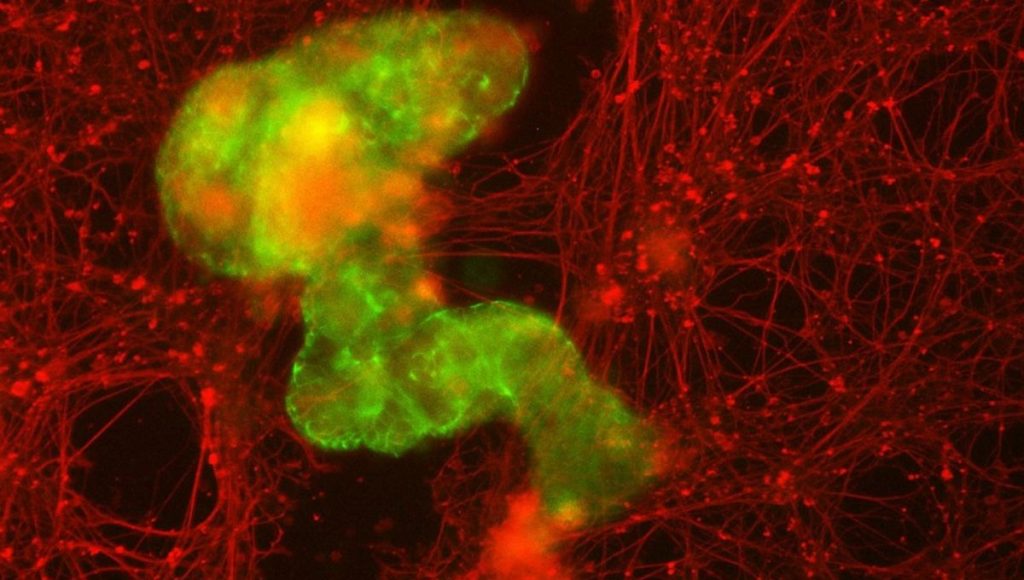
The starting point for the newest robots, called anthrobots, is a single adult human cell taken from the trachea (windpipe). These types of cells are covered in tiny hair-like structures called cilia which help keep tiny particles out of our lungs. By manipulating their growth conditions in the lab, the team was able to encourage the cells to replicate into multicellular organoids with the cilia facing outwards.
Now, with their coating of oar-like cilia beating away, the cells would be able to move.
In this colorized image, you can see the furry coating of cilia on the Anthrobot’s surface.
Image credit: Gizem Gumuskaya, Tufts University
A few different variants of the anthrobots emerged, with slightly different shapes and ranging in size between 30 and 500 micrometers. Depending on the arrangement of their cilia, they moved differently – wiggling around, traveling in straight lines, or moving in circles. They can survive in the lab for up to 60 days before naturally degrading.
This ability to spontaneously form their own shape is one of several advantages of the anthrobots.
“Unlike Xenobots, they don’t require tweezers or scalpels to give them shape, and we can use adult cells – even cells from elderly patients – instead of embryonic cells,” explained their creator, PhD student Gizem Gumuskaya, in a statement. “It’s fully scalable – we can produce swarms of these bots in parallel, which is a good start for developing a therapeutic tool.”
One of these potential therapeutic applications is in healing. The team observed that when a cluster of anthrobots (called a “superbot”) was added to neurons grown in the lab, which had been damaged by scratching the layer of cells, the miniature marvels encouraged new cell growth to fill in the gap.
And remember, the anthrobots are made of tracheal cells, not neurons. The scientists were surprised at their capabilities, which open up a whole host of potential applications in neurological diseases, tissue damage, and drug delivery. The fact that the cells naturally grow into such a range of structures, and that you could theoretically harvest a patient’s own cells for the process, thus limiting the chances of adverse immune reactions, means that we’re probably only scratching the surface of the possibilities.
“Two important differences from inanimate bricks are that cells can communicate with each other and create these structures dynamically, and each cell is programmed with many functions, like movement, secretion of molecules, detection of signals, and more,” Gumuskaya said. “We are just figuring out how to combine these elements to create new biological body plans and functions – different than those found in nature.”
“The cellular assemblies we construct in the lab can have capabilities that go beyond what they do in the body,” added senior author Michael Levin, director of the Allen Discovery Center at Tufts University.
“It is fascinating and completely unexpected that normal patient tracheal cells, without modifying their DNA, can move on their own and encourage neuron growth across a region of damage. We’re now looking at how the healing mechanism works, and asking what else these constructs can do.”
The study is published in the journal Advanced Science.